Is it just a sprained ankle?
If you work with a team, cater towards athletes, or are an active individual yourself, you’ve probably come across lateral ankle sprains - which is one of the most commonly injured parts of the body. All the more reason to step up and be at the top of your game when you have to evaluate one.
Looking back, I can tell you that in my haste (or arrogance), I’ve immediately thought of the anterior talofibular ligament (ATFL) being the damaged tissue, especially if someone points to the outer part of their ankle. It is widely accepted to be the most commonly injured ankle ligament, so why not play the odds? If I had to forecast and put money on it, I’d put it on an injured ATFL, wouldn’t you?!
I’m probably not the only one that has had this thought. I’ll bet that that’s what the majority of the clinicians and evaluators have thought and assumed … but if you think about it … why would you assume like the average clinician? I know you are more than the average health care provider who falls motionlessly within the mundane audience of the majority. Instead, you are one that will go the extra mile past what the majority of folks will do to figure out exactly what’s going on.
I’ll share just a couple quick tips that can boost you past your own menace of mediocrity so you can improve your clinical skills, or at least refresh any mental mind blocks!! Don’t be quick to judge a lateral ankle complaint without first considering these steps. Here are some quick checks that have added value to my diagnostic skills, that I hope will upgrade your clinical swag as well:
Palpate
First and foremost, rule out whether you have something that you can’t work on …. like a fracture. Assess these common fracture sites, and and observe for these findings prior to investigating further into your evaluation. If one or more of these check points are positive, it’s best to rule out a disruption in the osseous structures. The Ottawa Ankle Rules have been widely accepted as a guide to dictate whether or not radiographs should be performed.
OTTAWA ANKLE RULES (BMJ 2003)
Clear out these 5 things off your list first:
Posterior medial malleolus (from malleolus up shaft 6 cm)
Posterior lateral malleolus (from malleolus up shaft 6 cm)
Navicular (personally, I also assess the other tarsal bones too)
Base of 5th metatarsal (fibularis brevis avulsion fracture site)
Inability to bear weight
Any positive findings warrant radiographs
Standard ankle x-rays views contain: A-P, medial oblique, and lateral
TIP: If it’s in your scope of practice, get the mortise view also because it’ll help visualize other potential insults that the other views cannot capture well, especially within the talocrural junction.
STAR PLAYERS (most likely structures everyone pays attention to):
ATFL pathology
The most commonly injured ankle ligament
Calcaneofibular ligament (CFL) pathology
The 2nd most commonly injured ankle ligament
Interosseous ligament pathology
The 2nd most commonly injured syndesmotic ligament
This is where folks usually palpate for suspected high ankle injuries
BENCH PLAYERS (guys you think don’t matter, but are key fixtures):
Fibular shaft
Check for disruption or tenderness
Upper fibular shaft think: Maisonneuve fracture
Syndesmosis disruption + spiral fibular fracture
Spiral fracture at the proximal third of fibular shaft
Lower fibular shaft think: Dupuytren’s fracture
A fracture of the distal fibula shaft above the lateral malleolus
Can be associated with medial malleolar disruptions, ligamentous tears, or talar dislocations
Anterior Mortise
Check for disruption or tenderness
Distal anterior tibia think: Tillaux fracture
A growth plate fracture reserved for the young teens
Proximal talus think: talar dome lesion
Osteochondral intrarticular lesion in young adults to adults (teens - 30’s)
Occurs in 6% of all ankle sprains
Suspect if ankle sprain isn’t improving with conservative treatment
Lateral talus think: Snowboarder’s fracture
Mistaken for simple ankle sprain
Fracture at the lateral process of talus
Anteriolateral lesions of the ankle
ATFL’s Close Roommate
Anterior inferior tibiofibular ligament (AITFL) pathology
Commonly mistaken for the ATFL due to it’s close proximity to it
#1 most commonly injured syndesmostic ligament
Must differentiate between the ATFL
If disrupted, this is considered a “high ankle sprain”
Treatment and rehabilitative methods will vary from the simple ankle sprain
Recovery time will take longer from that of a simple “low ankle sprain”
Weight bearing x-rays (if possible) are necessary to rule out diastasis (gapping of bone) and instability
NOTE: In children, the AITFL remains intact; however, the ligament will pull on its tibial attachment site giving way to a growth plate fracture (aka. Tillaux fracture)
As you can see, both the Star Players and Bench Players play a significant part of any ankle evaluation. Just like in championship teams, all the team members are individually important as they collectively add value. Devaluing one or more player will most likely result in a disruption in unity, resulting in inadequate outcomes. Likewise, any negligence in assessing and oversight in palpating both the Star and Bench Players will compromise your ability to serve the injured individual properly. So you have to ask yourself, are you just catering to the star players, or is the whole team taken care of?
Once you thoroughly assess and get an idea of what structure(s) are involved, the inventory will help you formulate the possible mechanism of injury. Let’s take a dive into it now.
Mechanism Of Injury
Besides being a palpation phenom, knowing the mechanism of injury (MOI) is the other quick check I like to use when figuring out what injury an individual presenting with. The MOI will direct your focus and give you an idea of what structure is damaged. Depending on what particular insult was created during the movement, you can direct your attention and confirm the tissue(s) involved. The combination of palpatory findings along with the known MOI will automatically heighten the suspicion of what the athlete is suffering.
Here are some possible MOI, and the possible insulted structure:
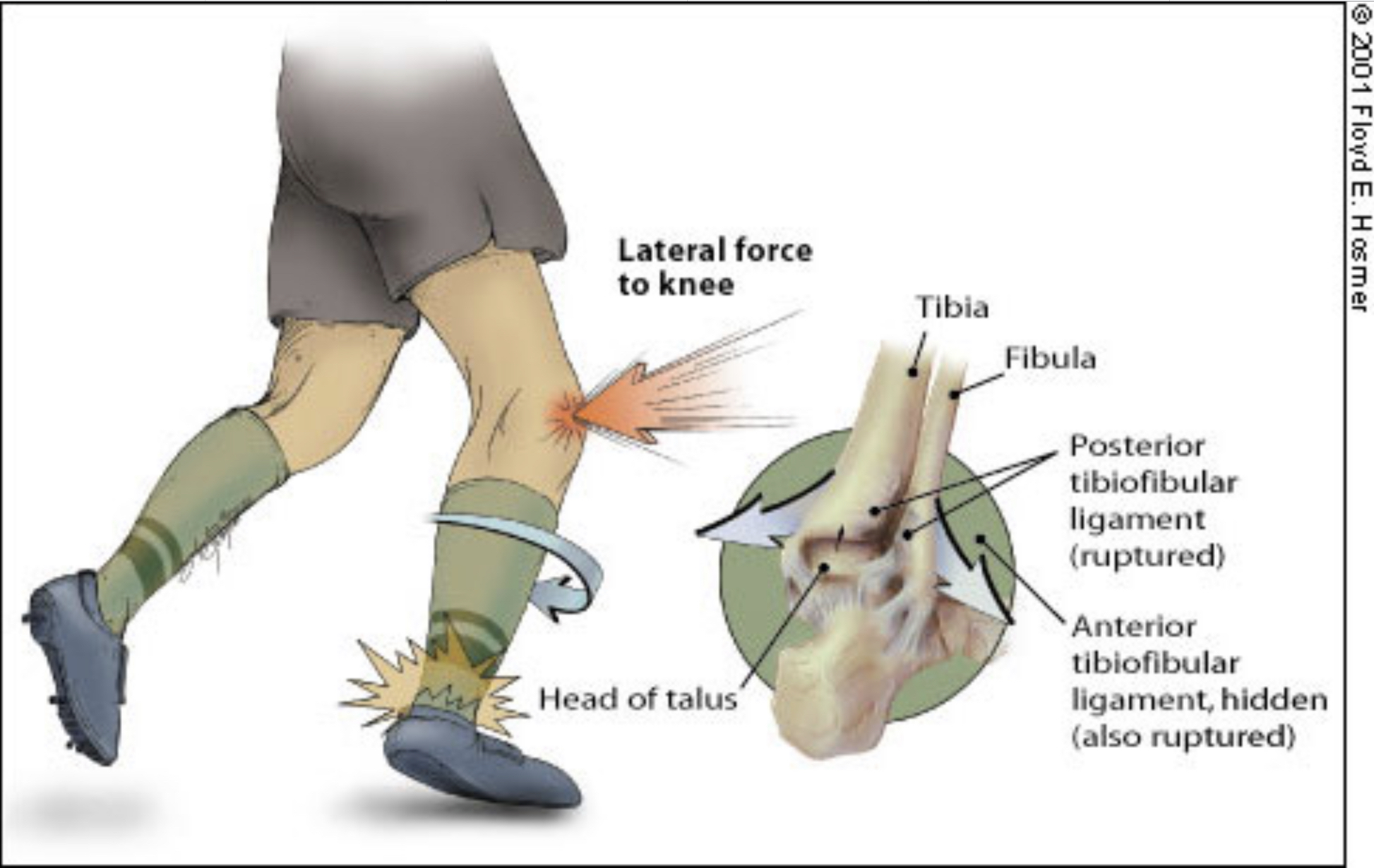
INVERSION + PLANTAR FLEXION
Anterior talofibular ligament (#1 most common injured ligament in low ankle sprain)
INVERSION
Calcaneofibular ligament (#2 most common injured ligament in low ankle sprain)
MOI: Inversion + Plantar Flexion
PLANTAR FLEXION
Posteromedial talar dome lesion - talus strikes tibia (#1 most common talar dome lesion)
INVERSION + DORSIFLEXION
Anterolateral talar dome lesion - talus strikes fibula (#2 most common talar dome lesion)
Talar Dome Lesion sites
EVERSION + DORSIFLEXION + EXTERNAL ROTATION (or combination of..)
Fibular pathology
Maisonneuve fracture (upper fibular shaft)
Dupuytren’s fracture (lower fibular shaft)
Syndesmosis
AITFL (#1 most common injured sydesmotic ligament in high ankle sprain)
Interosseous ligament (#2 most common injured ligament in high ankle sprain)
Tibial pathology
Tillaux fracture (seen in children)
Talar pathology
Snowboarder’s fracture
MOI: Eversion + Dorsiflexion + External Rotation
The great thing is, if you know only one of these (MOI or palpatory findings), then you can usually identify the other. Typically, the athlete/individual doesn’t know how their foot and ankle were positioned during the exact moment that they got injured, so be keen to rely heavily upon palpatory findings to give you the MOI. Adversely, if you’re out on the field and witnessed the actual MOI, then you can immediately formulate what structures are possibly harmed.
If both the MOI and palpatory findings are known, then you can solidify the results with provocative test and imaging (if necessary). Those additional tests can validate your suspicion of insulted tissues, and at the same time, help you prune your treatment plan.
Now, there you have it. Some clinical tips that I use when I’m looking at an ankle pathology! Hope this information buffs up your clinical skills and adds more swagger to your evaluation game!
Thanks for being curious and taking the time to read this! Hope it added value to your life and equips you to become better than you were yesterday!
Dr. Joe Jaime, DC, DACBSP®, ATC, CSCS®, FRC®ms, CES
Credit:
Anatomy extracted from the Visual Body app
Inversion MOI picture
Talar Dome Lesion picture
Eversion + DF + ER MOI picture