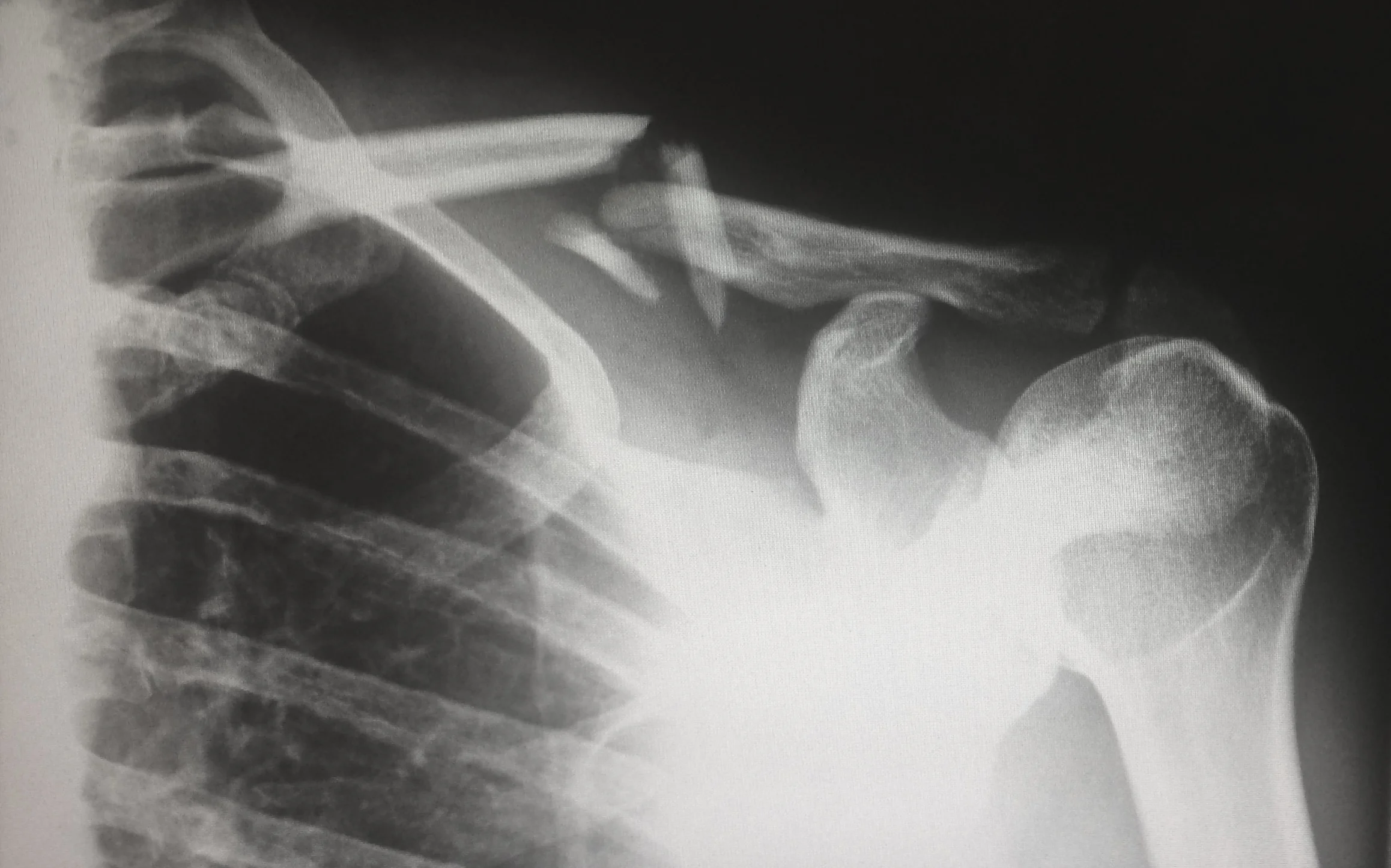
Typically, x-rays are the initial preference for imagining when the general population or amateur athlete gets injured. Not only is it fairly affordable (and something insurances won't typically having issues reimbursing), but it’s fast and easy to perform, and provides preliminary information on the integrity of the osseous structures. Whether bone disruption is a traumatic fracture, or progressive bone growth, radiographs are readily available and provide useful information.
DID YOU KNOW …
The one thing that you may not know is that it takes anywhere between 30-50% of osseous change before it will be visualized on radiographs. Basically that means your athlete’s questionable tibial shaft fracture has to be 30-50% “broken” before x-rays will even show it, and the occult osteochondroma that the youngster you’ve been treating will not show itself until 30-50% of the osseous integrity has been compromised!
This is why with questionable fracture, repeat x-rays may be taken 10-14 days later. It’ll either show a distinct radiolucent line (i.e. fracture), or visualize bone reabsorption (i.e. the white “healing” line indicating that there was a fracture).
The next time you get radiographs and it shows up negative, and you’re still iffy about what your dealing with, error more towards the side of caution. Taking it a step further, you may even want to investigate into getting advanced imaging (e.g. MRI, CT, etc.) or supplemental lab work (e.g. CBC, BMP/CMP, etc.). Use best judgement and your intuition, because not only is it good practice with your license/certification on the line, but most importantly, it is someone’s life that is entrusted to you.
Change your mindset … Change your perspective … life is much better when you have an
outlook that creates opportunity.
Thanks for being curious and taking the time to read this! Hope it added value to your life and equips you to become better than you were yesterday!
Dr. Joe Jaime, DC, DACBSP®, ATC, CSCS®, FRC®ms, CES
Source:
Harris WH, Heaney RP. Skeletal Renewal and Metabolic Bone Disease. N Engl J Med 1969; 280:303–311.